Julian Ellis OBE, M.Phil, C.Text, FTI, MRSC, MAE
Ellis Developments Ltd
Far Close, Rolleston Road, Fiskerton, Southwell, NG25 0UJ, UK
+44 (0) 7976 425899
www.ellisdev.co.uk
Info@ellisdev.co.uk
Ellis Developments Limited
Nottinghamshire, United Kingdom
| Surgical Implants |
| Textile Technology |
| Dt Michelle Rae |
| Julian Ellis Short CV |
| Consultancy |
| Contact Us |
| For sale |
| Shoulder Surgery |
| Vascular Surgery |
| Embroidered Surgical implants |
| Spider-Like Silk |
| Clavicle Replacement |
| Humerus Replacement |
| Nottingham Hood |
| Rotator Cuff Repair |
| Abdominal Aortic Aneurysms |
| Embroidered implant Project Report |
| Implant Picture Gallery |
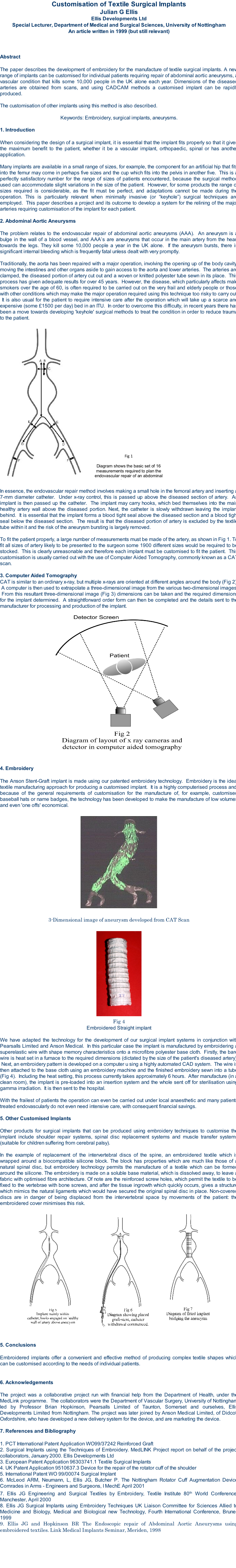
| Customisation of Surgical Implants |
| Embroidery |
| Through Stitching |
| Training and Quality Systems |
| Flammability |
| Composites |
| Engineering Textiles |
| Embroidery |
| Garment Quality |
| Fabric Quality |
| Dimensions |
| Instructors Courses |
| Knitting Operatives Course |
| Warp Knit inspection |
| Double Jersey Knitting Mechanics |
| V Bed Mechanics |
| Z-Axis Stitching |
| Embroidery for Composites |
| Structural Health Monitoring |
| Node and Truss Structures Project |
| Academic Report |
| Embroidery |
| Julian Ellis Full CV |
| About Julian Ellis |
| How to Find Us |
| Embroidered implant Project Report |
| Implant Picture Gallery |
| Customisation of Surgical Implants |